What is rheumatoid arthritis?
Watch our video about what rheumatoid arthritis is
Click to watch our short animation to find out what rheumatoid arthritis is, what the treatment options are and what you can do to help yourself.
Watch this video with other language subtitles
| Waa maxay xanuunka difaaca jirka ee saameeya kala-goysyada? | Somali subtitles |
| રૂમટોઈડ આર્થરાઈટિસ (Rheumatoid arthritis) એ શું છે? | Gujarati subtitles |
| முடக்கு வாதம் என்றால் என்ன? | Tamil subtitles |
| رہیموٹائیڈ آرتھرائیٹس (گٹھیا) کیا ہوتا ہے؟ | Urdu subtitles |
| Beth yw arthritis gwynegol? | Welsh subtitles |
Rheumatoid arthritis is a condition that can cause pain, swelling and stiffness in joints.
It is what is known as an auto-immune condition. This means that the immune system, which is the body’s natural self-defence system, gets confused and starts to attack your body’s healthy tissues. In rheumatoid arthritis, the main way it does this is with inflammation in your joints.
Rheumatoid arthritis affects around 400,000 adults aged 16 and over in the UK. It can affect anyone of any age. It can get worse quickly, so early diagnosis and intensive treatment are important. The sooner you start treatment, the more effective it’s likely to be.
To understand how rheumatoid arthritis develops, it helps to understand how a normal joint works.
How does a normal joint work?
A joint is where two bones meet. Most of our joints are designed to allow the bones to move in certain directions and within certain limits.
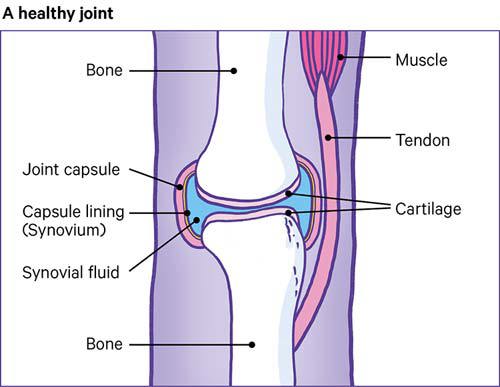
For example, the knee is the largest joint in the body and one of the most complicated. It must be strong enough to take our weight and must lock into position, so we can stand upright.
It also has to act as a hinge, so we can walk, and needs to twist and turn when we run or play sports.
The end of each bone is covered with cartilage that has a very smooth, slippery surface. The cartilage allows the ends of the bones to move against each other, almost without rubbing.
The joint is held in place by the synovium, which contains thick fluid to protect the bones and joint.
The synovium has a tough outer layer that holds the joint in place and stops the bones moving too far.
Strong cords called tendons anchor the muscles to the bones.
What happens in a joint affected by rheumatoid arthritis?
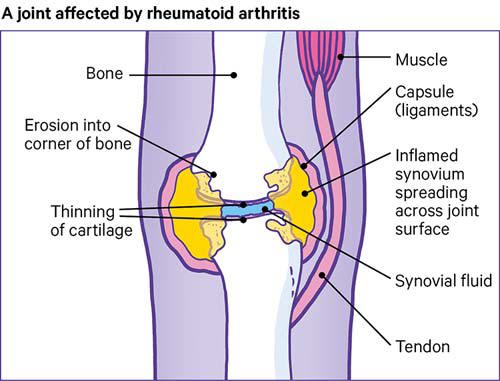
If you have rheumatoid arthritis, your immune system can cause inflammation inside a joint or a number of joints. Inflammation is normally an important part of how your immune system works. It allows the body to send extra fluid and blood to a part of the body under attack from an infection. For example, if you have a cut that gets infected, the skin around it can become swollen and a different colour.
However, in the case of rheumatoid arthritis, this inflammation in the joint is unnecessary and causes problems.
When the inflammation goes down, the capsule around the synovium remains stretched and can’t hold the joint in its proper position. This can cause the joint to become unstable and move into unusual positions.
Symptoms
The main symptoms of rheumatoid arthritis are:
- joint pain
- joint swelling, warmth and redness
- stiffness, especially first thing in the morning or after sitting still for a long time.
Other symptoms can include:
- tiredness and lack of energy – this can be known as fatigue
- a poor appetite (not feeling hungry)
- weight loss
- a high temperature, or a fever
- sweating
- dry eyes – as a result of inflammation
- chest pain – as a result of inflammation.
Rheumatoid arthritis can affect any joint in the body, although it is often felt in the small joints in the hands and feet first. Both sides of the body are usually affected at the same time, in the same way, but this doesn’t always happen.
A few people develop fleshy lumps called rheumatoid nodules, which form under the skin around affected joints. They can sometimes be painful, but usually are not.
Causes
The following can play a part in why someone has rheumatoid arthritis:
Age
Rheumatoid arthritis affects adults of any age, although most people are diagnosed between the ages of 40 and 60.
Around three-quarters of people with rheumatoid arthritis are of working age when they are first diagnosed.
Sex
Rheumatoid arthritis is two to three times more common among women than men.
Genetics
Rheumatoid arthritis develops because of a combination of genetic and environmental factors, such as smoking and diet. It is unclear what the genetic link is, but it is thought that having a relative with the condition increases your chance of developing the condition.
Weight
If you are overweight, you have a significantly greater chance of developing rheumatoid arthritis than if you are a healthy weight.
The body mass index (BMI) is a measure that calculates if your weight is healthy, using your height and weight.
For most adults, an ideal BMI is in the 18.5 to 24.9 range.
If your BMI is:
- below 18.5 – you're in the underweight range
- between 18.5 and 24.9 – you're in the healthy weight range
- between 25 and 29.9 – you're in the overweight range
- between 30 and 39.9 – you're in the obese range.
To work out your BMI, use the healthy weight calculator.
Smoking
Cigarette smoking significantly increases the risk of developing rheumatoid arthritis. If you would like to stop smoking, visit the Smokefree website.
Diet
There is some evidence that if you eat a lot of red meat and don’t consume much vitamin C, you may have an increased risk of developing rheumatoid arthritis.
How will rheumatoid arthritis affect me?
Because rheumatoid arthritis can affect different people in different ways, we can’t predict how the condition might develop for you.
If you smoke, it’s a very good idea to quit after a diagnosis of rheumatoid arthritis. This is because:
- rheumatoid arthritis may be worse in smokers than non-smokers
- smoking can weaken how well your medication works.
Physical activity is also important, as it can improve your symptoms and benefit your overall health.
Blood tests and x-rays will help your doctor assess how fast your arthritis is developing and what the outlook for the future may be. This will also help your doctor to decide which form of treatment to recommend.
The outlook for people with rheumatoid arthritis is improving all the time, as new and more effective treatments become available. It is possible to lead a full and active life with the condition, but it is important to take your medication as prescribed and make necessary lifestyle changes.
Diagnosis
A diagnosis of rheumatoid arthritis is based on your symptoms, a physical examination and the results of x-rays, scans and blood tests.
It can be difficult to diagnose because there isn't a test that can prove you definitely have it. There are also quite a few conditions that have the same symptoms.
Your doctor will ask about your symptoms and do a physical examination. They will look for swollen joints and check how well your joints move. Rheumatoid arthritis can affect different parts of your body at once, so it's important to tell your doctor about all the symptoms you've had, even if they don't seem to be related.
If they think you have rheumatoid arthritis, they will refer you to a rheumatologist and may arrange blood tests to help confirm a diagnosis.
Blood tests
There's no single blood test that can confirm you have rheumatoid arthritis. However, there are a few tests that can show possible signs of the condition. Some of the main tests are outlined below.
Erythrocyte sedimentation rate (ESR)
A sample of your red blood cells are put into a test tube of liquid. The cells are timed to see how long they take to get to the bottom of the tube. If the cells sink faster than usual, you may have levels of inflammation that are higher than normal. Rheumatoid arthritis is just one possible cause.
C-reactive protein (CRP)
This test can show if there is inflammation in your body. It does this by checking how much CRP there is in your blood. If there is more CRP than usual, you may have inflammation in your body.
Full blood count
A full blood count measures the number of red blood cells you have. These carry iron around your body, and a low number of red blood cells means you have a low iron content. This may mean you have anaemia (an-ee-me-er) and is common in people with RA, although having anaemia doesn't prove you have RA.
Rheumatoid factor and anti-CCP antibodies
About half of all people with rheumatoid arthritis have rheumatoid factor in their blood when the condition starts. However, around 1 in every 20 people without rheumatoid arthritis also test positive for rheumatoid factor.
There is another antibody test called anti-CCP that you can take. People who test positive for anti-CCP are very likely to get rheumatoid arthritis. However, not everyone that has the condition has this antibody.
Scans
Scans may be used to check for joint inflammation and damage. These can be used to diagnose rheumatoid arthritis and to check how the condition is developing.
These may include:
- x-rays – these will show any changes in your joints
- ultrasound scans – a picture of your joints is created using high-frequency sound waves
- magnetic resonance imaging (MRI) scans – pictures of your joints are produced using strong magnetic fields and radio waves.
Treatment
There are a variety of treatments available for rheumatoid arthritis. The earlier that intensive treatment is started, the more likely it is to work.
There are three main ways to treat rheumatoid arthritis:
- drugs
- physical therapies
- surgery
Drugs
There are four main groups of drugs that are used to treat rheumatoid arthritis. These are:
- painkillers
- non-steroidal anti-inflammatory drugs (NSAIDs)
- disease-modifying anti-rheumatic drugs (DMARDs)
- steroids (also known as corticosteroids).
Many people with rheumatoid arthritis need to take more than one drug. This is because different drugs work in different ways.
Your drug treatments may be changed from time to time. This can depend on how bad your symptoms are, or because something relating to your condition has changed.
Drugs may be available under several different names. Each drug has an approved name – sometimes called a generic name.
Manufacturers often give their own brand or trade name to the drug as well. For example, Nurofen is a brand name for ibuprofen.
The approved name should always be on the pharmacist’s label, even if a brand name appears on the packaging. Check with your doctor, rheumatology nurse specialist or pharmacist if you’re not sure about anything.
Painkillers
Painkillers can help to relieve the pain caused by rheumatoid arthritis, but should not be the only treatment used.
There are many types and strengths of painkillers available – some can be bought over the counter from a pharmacy, while some are only available on prescription.
For guidance, ask a healthcare professional in charge of your care.
Disease-modifying anti-rheumatic drugs (DMARDs)
There are three types of DMARD:
- conventional synthetic DMARDs (sometimes called csDMARDs)
- biological therapies (sometimes called bDMARDs).
- targeted synthetic DMARDs (sometimes called tsDMARDS).
You will need to have regular blood tests if you take DMARDs, as they can affect your liver.
It may be a while before you notice your DMARD working – possibly a few months. It is important to keep taking your medication during this time.
The table below shows the DMARDs available for the treatment of rheumatoid arthritis.
| Name | Type of DMARD |
|---|---|
| Azathioprine | Conventional synthetic DMARD |
| Hydroxychloroquine | Conventional synthetic DMARD |
| Leflunomide | Conventional synthetic DMARD |
| Methotrexate | Conventional synthetic DMARD |
| Sulfasalazine | Conventional synthetic DMARD |
| Etanercept | Biologic; Anti-TNF |
| Infliximab | Biologic; Anti-TNF |
| Rituximab | Biologic; Anti lymphocyte monoclonal antibody |
| Baricitinib | Targeted synthetic DMARD |
| Tofacitinib | Targeted synthetic DMARD |
| Sarilumab | Biologic: Anti IL6 |
| Certolizumab pegol | Biologic; Anti-TNF |
| Adalimumab | Biologic; Anti-TNF |
| Golimumab | Biologic; Anti-TNF |
| Abatacept | Biologic T cell co-stimulator |
| Tocilizumab | Biologic; Anti IL6 |
For more information on the types of drugs used to treat rheumatoid arthritis, see our drugs content.
Steroids
Steroids are sometimes known by their full name: corticosteroids.
Corticosteroids help to reduce the pain, stiffness and inflammation caused by rheumatoid arthritis.
They can be used as:
- a tablet
- an injection directly into a painful joint
- an injection into your muscle.
They're usually used to provide short-term pain relief. This could be during a flare-up or while you're waiting for your DMARD medication to start working.
Corticosteroids are normally only used in this way because long-term use of corticosteroids can have serious side effects, including weight gain, osteoporosis and thinning of the skin.
You shouldn’t stop taking your steroid tablets or alter the dose unless advised to by your doctor. It can be dangerous to stop steroids suddenly.
Non-steroidal anti-inflammatory drugs (NSAIDs)
NSAIDs can be used to help control symptoms of pain, swelling or stiffness. They can be used in combination with painkillers.
NSAIDs start working within a few hours, with the effects felt for a few hours to a whole day.
Ibuprofen is a commonly prescribed NSAID.
NSAIDs can be taken as a:
- tablet
- capsule
- liquid
- suppository to be inserted into your bum
- cream
- gel.
Managing symptoms
Managing a flare-up
When your symptoms get worse, this is known as a flare-up. These can happen at any time, but can happen after you have been stressed or had an infection.
Over time, you may get better at noticing the early signs of a flare-up.
If you’re having regular flare-ups, you should mention this to your doctor. It may be that you need to review your treatment.
Here are a few things you can do to help yourself during a flare-up:
- Keep taking your medication at the doses you’ve been prescribed.
- Do gentle exercises.
- Put heated items on the joint – these can include a hot water bottle or electric heat pad. See below for more information.
- Put cold items on the joint – these can include a bowl of cold water with ice cubes, a pack of frozen peas wrapped in a towel, or a damp towel that has been kept in the fridge. See below for more information.
- Let people around you know, so they can help and support you.
Tips for using heated items
Heated items that could help your joint pain include a hot water bottle or electric heat pad. Wrap these in a towel, then place on a painful joint. You could also try having a hot or warm shower or bath.
Other heated items that people have found useful are wheat bag, heat pads, deep heat cream, or a heat lamp.
Make sure these items are warm but not hot, as you could risk burning or scalding yourself. Gentle heat will be enough.
A towel should be placed between the heated item and the skin for protection. Check your skin regularly, to make sure it is not burning.
Tips for using ice packs
Some people find that using an ice pack can help their joint pain. You can buy one from a pharmacy, or you can make one at home, by wrapping ice cubes in a plastic bag or wet tea towel.
Here’s how to apply the ice to your skin:
- Rub a small amount of oil over where you’d like the ice pack to go. Any type of oil can be used. If your skin is broken – for example, if you have a cut – don’t use the oil and cover the area with a plastic bag. This will stop the cut getting wet.
- Put a cold, wet flannel over the oil.
- Put the ice pack over the flannel and hold it there.
- After five minutes, check the colour of your skin. Remove the ice pack if your skin has turned bright pink or red. If it hasn’t, leave it on for another 5 to 10 minutes.
- You can leave the ice pack on for 20-30 minutes. Don’t leave it on for any longer, as you could damage your skin if it is left on for too long.
Physical activity
Keeping physically active can improve your rheumatoid arthritis symptoms, including pain.
You may find it difficult to be physically active in the first place, especially if you are having a flare-up. However, if you find the right activities, help and support, you can be active in a way that suits you.
Not keeping active can lead to stiff joints and weak muscles. It could also cause you to gain weight.
If you are new to exercise, or haven’t exercised in some time, you may feel a bit sore the first few times you try a new activity. As you get used to it, this will get better.
However, if a type of exercise always causes a flare-up, it's probably best to find another one. High-impact exercises such as step exercises, or contact sports, such as rugby and football, are more likely to cause problems. Swimming, walking, gentle cycling and aqua aerobics generally put less strain on your joints.
Yoga and tai chi are generally thought to be suitable for those with rheumatoid arthritis. However, there are many different styles, so it is best to check the style is suitable for your condition before you sign up to a class.
You should also break up long periods of sitting with light activity, to avoid being sedentary for extended periods.
Physiotherapy
A physiotherapist can suggest suitable exercises for you and support you in keeping active.
People with rheumatoid arthritis should have access to specialist physiotherapy to help manage their condition and improve their fitness, flexibility and strength. You should also have follow-up reviews.
Find a physiotherapist on The Chartered Society of Physiotherapy website.
Hydrotherapy
You may also find that hydrotherapy helps to ease your symptoms. This involves doing special exercises in a warm-water pool, under the supervision of a trained physiotherapist. Hydrotherapy can also be called ‘aquatic therapy’ or ‘aquatic physiotherapy’.
Any member of your healthcare team should be able to refer you to an NHS physiotherapist if they think you might benefit from hydrotherapy. In some parts of the UK, you can also refer yourself to a physiotherapist, who will assess whether hydrotherapy would be suitable for you.
Check with your GP or call your local rheumatology department to find out if an NHS physiotherapist in your area will accept self-referrals.
You can also choose to use private healthcare, but it’s important to be aware that in rare instances, private hydrotherapy may be unregulated, and so the quality of the changing areas, the water or general environment can vary.
Check before your treatment starts that you’re happy with the facility. A qualified physiotherapist will be registered with the Health & Care Professions Council (HCPC).
It’s also recommended that you see someone who’s a member of the Chartered Society of Physiotherapists (CSP) and who’s accredited by the Aquatic Therapy of Chartered Physiotherapists (ATACP).
It can help to improve the pain in your joints, and you may also find it relaxing. Ask your doctor or physiotherapist if they think hydrotherapy would be suitable for you.
Foot problems
Foot problems for those with rheumatoid arthritis include:
- pain
- soreness
- warmth and swelling that lasts at least a few days
- the foot changing shape
- difficulty walking
- your shoes rubbing
- corns or calluses, and nail problems
- Infections such as athletes foot, verruca or bacterial infections.
If these problems are left untreated, they can lead to the infections spreading and, eventually, to ulcers forming.
It is therefore important to see a podiatrist, who specialises in general foot care. They can give advice on footwear, information on how to treat foot problems yourself, and can provide special insoles. They can also monitor your foot and general health, and will refer you to a consultant if they find any issues.
There may be a podiatrist in the rheumatology department where you receive your care, or you may get a referral to an NHS podiatrist. GPs can also refer you to community-based services.
Alternatively, you can access podiatry care privately.
You can find a private podiatrist on the College of Podiatry website. All podiatrists should be registered with the Health & Care Professions Council (HCPC).
Complementary treatments
Complementary treatments can be useful when used alongside prescribed medicines for the treatment of rheumatoid arthritis. However, they should not replace your prescribed medicines and you should talk to your rheumatology team before starting a complementary treatment.
Generally complementary treatments aren't considered to be evidence-based and are therefore not usually available on the NHS.
Living with rheumatoid arthritis
Occupational therapy
Occupational therapists can help you keep doing the activities you need or want to do – at home or at work. They will work with you to find different ways of doing things.
The benefits of seeing an occupational therapist include:
- improved confidence
- being able to do more things, at home or at work
- being able to live independently at home
- allowing you to return to or stay in work.
Ask your GP about occupational therapists that are local to you. If you regularly see a social worker, nurse or other health care professional, they can help you contact an occupational therapist through health or social services.
Be prepared to describe any difficulties you have and how they are affecting your life, or the lives of those who care for you.
You may want to know how long it will be until you get an appointment, so remember to ask if there is a waiting list.
You can also see an occupational therapist privately. You will be able to get an appointment quicker, but it will cost you money.
Find an occupational therapist that works privately on the Royal College of Occupational Therapist website. All occupational therapists should be registered with the Health & Care Professions Council (HCPC).
Occupational therapy
Occupational therapists can help you keep doing the activities you need or want to do – at home or at work. They will work with you to find different ways of doing things.
The benefits of seeing an occupational therapist include:
- improved confidence
- being able to do more things, at home or at work
- being able to live independently at home
- allowing you to return to or stay in work.
Ask your GP about occupational therapists that are local to you. If you regularly see a social worker, nurse or other health care professional, they can help you contact an occupational therapist through health or social services.
Be prepared to describe any difficulties you have and how they are affecting your life, or the lives of those who care for you.
You may want to know how long it will be until you get an appointment, so remember to ask if there is a waiting list.
You can also see an occupational therapist privately. You will be able to get an appointment quicker, but it will cost you money.
Find an occupational therapist that works privately on the Royal College of Occupational Therapist website. All occupational therapists should be registered with the Health & Care Professions Council (HCPC).
Aids and adaptations
If you have trouble doing everyday tasks, you may find it useful to use certain aids and adaptations.
Aids can help you manage everyday tasks such as bathing, dressing, and cooking. These can include shoe horns, rails or handles, and shower seats.
Adaptations are bigger items that can help you move around your home. These items include wheelchairs, fixed ramps and baths with built-in handles.
In England, local councils must provide aids and minor adaptations costing £1000 or less free of change to anyone with an eligible care need. Your council may call this ‘community equipment’.
You can also access adaptations that cost over £1000, but you must apply for these through a Disabled Facilities Grant.
You can request a needs assessment from your council to see if you would be eligible for aids and adaptations. You can apply for a needs assessment and find out more here: https://www.gov.uk/apply-needs-assessment-social-services
Aids and minor adaptations you receive form your local council should not be means-tested, meaning that no matter how much money you have, the local authority has to provide you with them.
If you live in Wales, Scotland or Northern Ireland, contact your GP or local council for information about access to these items.
Further support
If you are living with rheumatoid arthritis, you may also be living with one or more other conditions.
This is not unusual – 54% of those aged over 65 in England are living with two or more long-term conditions. Depression is the most common condition among people with rheumatoid arthritis, affecting one in six people.
If you are feeling low, talk to your GP, who can signpost you to the appropriate services. You can also call the arthritis helpline for free on 0800 5200 520, where our trained advisors can give you help and support. We’re open from 9am to 8pm, Monday to Friday, except for bank holidays.
If you're over the age of 55, The Silver Line is there 24 hours a day, 365 days a year to provide information, support and friendship.
If you're a man experiencing distressing thoughts and feelings, the Campaign Against Living Miserably (CALM) is there to support you.
If you identify as gay, lesbian, bisexual or transgender, Switchboard is available from 10am–11pm, 365 days a year, to listen to any problems you're having.
Surgery
Surgery is sometimes needed for those with rheumatoid arthritis. This can be to reduce pain, correct joint shape or restore your ability to use your joint. The types of surgery people with rheumatoid arthritis undergo are:
Foot Surgery
Examples of this type of surgery include:
- Removal of inflamed tissues around the joints of the forefoot.
- Removal of the small joints in the ball of the foot.
- Straightening of toes.
- Fixation of joints.
Finger, hand and wrist surgery
Examples of this type of surgery include:
- carpal tunnel release
- removal of inflamed tissue in the finger joints
- release of tendons in the fingers (this is used to treat unusual bending).
Arthroscopy
Arthroscopy is used to remove inflamed joint tissue.
During the operation, an arthroscope is inserted into the joint through a small cut in the skin, so the surgeon can see the affected joint. Damaged tissue is then removed. You usually don't have to stay overnight in hospital for this type of surgery, but the joint will need to be rested at home for several days.
Joint replacement
Some people with rheumatoid arthritis need surgery to replace part or all of a joint - this is known as a joint replacement, or arthroplasty. Common joint replacements include the hip, knee and shoulder.
Replacement of these joints is a major operation that involves several days in hospital, followed by rehabilitation, which can take months. The latest joints generally last for 10 to 20 years, and there is no guarantee that the new joint will be fully functional.
For more information on surgery, see our surgery content.
Diet and nutrition
There's no single diet that will help everyone with rheumatoid arthritis. However, some people find that making changes to their diet helps their symptoms.
For more information, see our diet and arthritis content.
Supplements
There is little evidence that taking supplements will improve rheumatoid arthritis, or its symptoms. However, some people think certain supplements work for them.
What is important is that you are not wasting your money on expensive supplements that won’t do anything for your condition.
Some supplements may be prescribed by your specialist team or GP. For example, folic acid may be prescribed if you are taking methotrexate, and calcium and vitamin D may be prescribed if you are taking steroids.
A healthy, balanced diet should contain all the vitamins and minerals you need.
However, it’s recommended that people should consider taking a daily supplement containing 10 micrograms of vitamin D in autumn and winter, as it is difficult to get the amount needed through sunlight at this time of year.
It’s also recommended that people whose skin has little or no exposure to the sun should take a vitamin D supplement throughout the year. This could include people in care homes and people who cover their skin when outside.
Ethnic minority groups with dark skin – from African, Afro-Caribbean and South Asian backgrounds – should also consider taking a supplement throughout the year, as they may not get enough vitamin D from sunlight in the summer.
Sleep
Getting a good night’s sleep can be tough, especially when you are living with the aches, pains and inflammation of rheumatoid arthritis.
For more information on how to get a good night’s sleep, see our Sleep and Arthritis booklet, or visit The Sleep Council website.
Sex and relationships
Most couples – whether they have arthritis or not – go through phases when their sex life is less exciting or satisfying than it was. There may be physical reasons for this, but emotional factors and stress often play a part.
Arthritis can present a number of challenges in a relationship, including the following:
- Pain and fatigue may reduce your enjoyment of sex, and other activities and interests that you share with your partner.
- Arthritis may mean that you can’t always manage the household jobs you usually do, or you may need help with them.
- If your arthritis affects your work, it may lead to financial worries.
- Having arthritis may affect your mood and self-esteem.
- Your partner will be concerned about how the condition is affecting you.
For more information, see our sex, relationships and arthritis content.
Research and new developments
Here, we round up some of the latest developments in rheumatoid arthritis research.
Our previous research has:
- led to the development of a new type of drug. These drugs are called ‘biological therapies’ and have transformed the lives of people with rheumatoid arthritis over the past 20 years.
- highlighted the importance of starting early, intensive treatment for inflammatory arthritis within 12 weeks of symptoms starting. It has also led to the introduction of a best practice tariff for those with rheumatoid arthritis, which means people are being diagnosed quicker.
We're currently funding research projects to find out what causes rheumatoid arthritis, and to develop new and improved treatments. For example:
- our centre for genetics and genomics is trying to understand how genetic factors determine whether certain people are at risk of developing inflammatory arthritis, and what happens when they do
- our rheumatoid arthritis pathogenesis centre of excellence is looking at why rheumatoid arthritis starts, why it attacks the joints, and why the inflammation carries on rather than switching off
- investigating how the organisms that live on our skin and in our gut differ in those with rheumatoid arthritis and how this affects a person’s response to treatment.
Keri's story

I was diagnosed with rheumatoid arthritis at the age of 21.
I was in my third year of university, studying to be a primary school teacher. Suddenly, one morning, my thumbs became very painful. Then my elbows became stiff and sore, and I couldn’t straighten my arms.
At first I only had symptoms in the morning, but eventually I had them all the time. Quite a few of my joints were stiff and painful, which meant I couldn’t get around very well. I was also tired a lot. When this happened, my GP referred me to a rheumatologist.
I graduated from my teacher training course two years later than planned, but have not been able to work as a teacher yet, due to my arthritis. However, I have used my teaching skills to volunteer for Versus Arthritis, leading self-management courses in Northern Ireland, which I find extremely enjoyable and rewarding. I am also the Chairperson of my local Versus Arthritis support group.
Baking is one of my hobbies, although using certain kitchen equipment can be difficult. Being social is important to me too and I enjoy going to cafés to catch up with my friends. When I’m in pain, I can distract myself by reading or listening to music.
Exercise is important to me too, as I find that doing some gentle exercises makes my joints less painful. There are a few chair-based exercises I do regularly and I also enjoy going for short walks.
Swimming is great too and I find that doing exercises in the heated water of the hydrotherapy pool makes me feel less stiff and sore.
Medication-wise, I’m currently using a biological injection called Enbrel. I’ve been using it for five years and inject myself once a week. It’s really helped to control my condition and my flare-ups happen less often.
At the moment, I’m doing ok. There are good days and bad days. I still experience pain every day, but am doing much better than when I was first diagnosed. I have fewer flare ups, which shows that the medication I’m using is really helping me.
My advice to anyone who has recently been diagnosed with rheumatoid arthritis would be to join a support group. Talking to another person who has the same condition as you and knows what you’re going through is really useful and reassuring. It’s helped me a lot in my journey.
I’d also say that getting a good night’s sleep is important, as it can help your body recover from the effects of your arthritis. It’s also important for me to learn more about my condition, as it helps me to understand what my body is going through. I really do believe that knowledge is power!
Phil's story

I was diagnosed with rheumatoid arthritis in 2006, as far as I can remember.
At the time I was doing what I do now, which is co-running a charity video production company, and living in South London with my (now late) wife, a dog and a parrot. I was living a fairly active life, playing badminton, sailing and trying to learn to ski.
My initial symptoms weren’t that bad, to be honest. There was some swelling in one finger that I went to the GP about, as it was impacting my work. It was on the little finger on my right hand, which, although it sounds minimal, was important in terms of the particular camera I was using at the time. Looking back though, there had been other shorter-term episodes where I had acute joint pain in hands and wrists, which I just put down to ongoing busy work.
I’m not currently on any medication, as my partner and I are trying for our second child. And being on no treatment is not working! I have quite a lot of pain, stiffness and am really tired at the moment, but hopefully this will only be for a short while. I’m taking NSAIDs and the occasional steroid injection to manage my symptoms.
My hobbies have definitely been impacted by having arthritis. I love sailing, but being able to manage ropes, helming and hanging on in a rough sea all require good grip strength. However, I find it’s about leaving a bit more time to do things and planning ahead.
Particularly if I’m single-handed on the boat, I’ll be more cautious about the forecast and plan accordingly.
I play badminton, although at the moment I’m finding my joints a bit too painful to play. I’m sure, compared to a similar person my age, I am slower in getting things done, or a bit more cautious about how I do it, but mostly it’s just a case of getting on with it and not fussing. I generally don’t speak about my arthritis, as I’m reasonably stubborn and hate the idea of being pushed around by something outside of my control. This can be to my detriment though, as sometimes I will just keep going and I’ll be exhausted the next day.
My advice to anyone who has been recently been diagnosed with rheumatoid arthritis is that your condition doesn’t define you. It’s very easy to let a diagnosis like this overshadow everything else, but it’s just a part of my life. Sometimes it will be a dominant part, but sometimes it will just be ticking along in the background.
I have also accepted that there will be a trade off. Although my symptoms and long-term effects can be managed, there are often side effects from the medications I use. There is no perfect solution, so I just accept this and crack on with life.